- Abstract
- Introduction
- The aim of this study was to compare the effects of Er:YAG laser and standard scalpel technique in treatment of gingival hyperpigmentation over a period of 6 months, regarding the efficacy of depigmentation and the stability of the results in the follow-up period, hemostasis effect, postoperative pain perception and discomfort, wound healing capacity, patient preference of the techniques, and the level of patient satisfaction after the therapy.
- Method and Materials
- Results
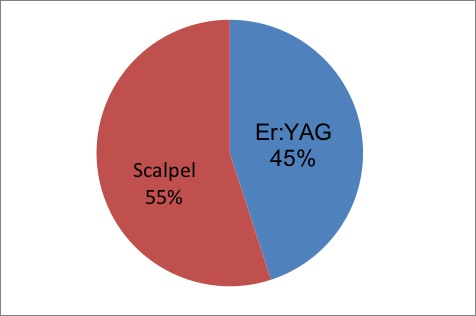
- A total of 20 subjects successfully completed the study period of 6 months and were included in the data analyses. All 20 participants maintained the recall visits at 2 and 6 months (Fig 2).
Gingival depigmentation using Er:YAG laser and scalpel technique: A six-month prospective clinical study
MedUP vetpool
Rola Alhabashneh, Obaida Darawi, Yousef S. Khader, Lama Ashour
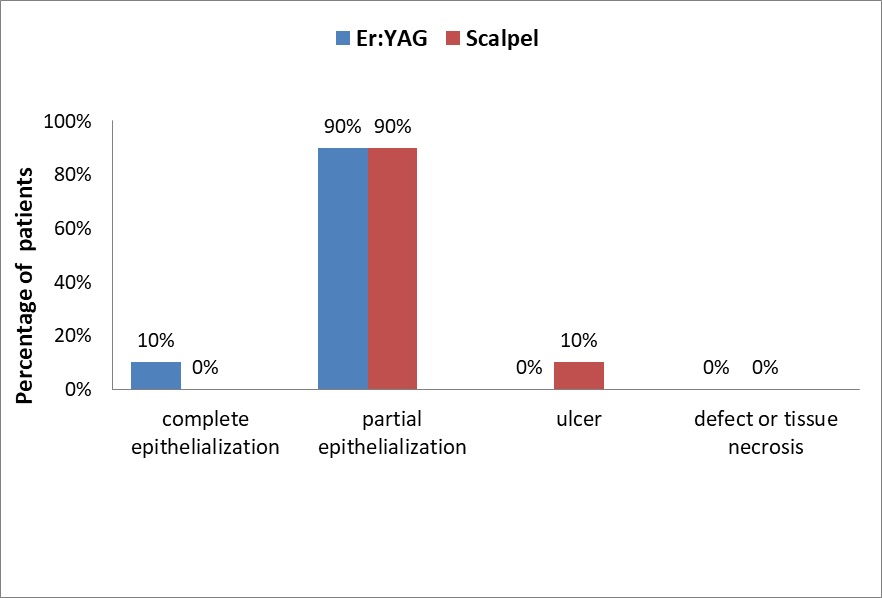
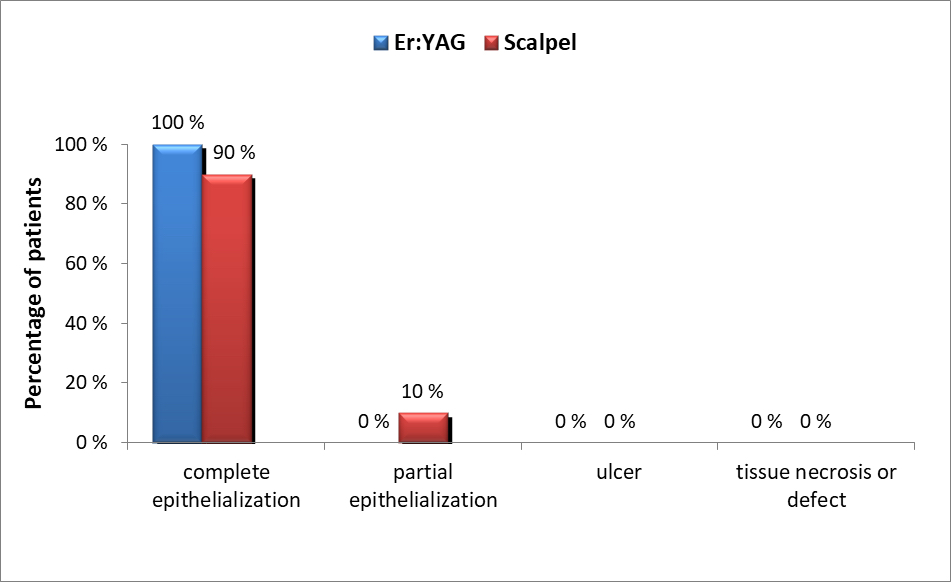
Objective : To compare the 6-month clinical efficacy of Er:YAG laser and standard scalpel technique in treating gingival hyperpigmentation. Method and Materials : Patients requesting treatment for moderate to severe gingival hyperpigmentation in the maxilla were enrolled in this split-mouth study. The contralateral maxillary sides were randomly assigned to receive either Er:YAG laser (continuous wavelength of 2,940 nm) with a noncontact tip or the standard scalpel technique. Dummett oral pigmentation index (DOPI) and Hedin melanin index (HMI) were compared at the baseline and at 1 and 2 weeks, and 1, 3, and 6 months following the treatment. Bleeding Index, total treatment time, patient preference, pain perception at the first 3 days, wound healing, and level of satisfaction were also compared. Mann-Whitney test, Kruskal-Wallis test, and chi-square test were used to test the significance between variables. A P value of less than or equal to .05 was considered statistically significant. Results: Of the 22 patients enrolled, 20 completed this study. After assessing DOPI and HMI at 1 and 2 weeks, and at 1-, 3-, and 6-month follow-up appointments, both Er:YAG laser and scalpel were significantly effective in treating gingival hyperpigmentation when compared to baseline ( P < .001) but with no statistically significant difference between the two treatment methods ( P > .05). More patients preferred the scalpel technique as it was associated with slightly shorter treatment time and less postoperative pain when compared to Er:YAG laser, but with no statistical significance ( P > .05). Er:YAG laser sites showed minimal bleeding and more rapid wound healing ( P < .001). Conclusion : Both Er:YAG laser and scalpel technique achieved similar outcomes regarding the efficacy of gingival depigmentation, postoperative pain perception, and the time required for the treatment. Laser therapy requires more advanced technology and is associated with higher financial costs. Therefore, the scalpel technique is still considered the gold standard treatment for gingival depigmentation.
- Keywords
- gingiva
- laser
- melanin
- depigmentation